
Breast Cancer
Breast cancer symptoms
Breast cancer does not always have symptoms, particularly in its earliest stages. At UCI Health, our breast cancer screening specialists detect most breast cancers through annual screening mammograms.
But if you have any of these signs of breast cancer, talk to your primary care doctor:
- A breast lump
- Breast pain that does not go away within a week or two
- Changes in the skin on your breast, including dimpling, redness or darkening
- Changes in the size or shape of your breast
- Nipple discharge
- An itchy rash on your nipple

Find a cancer clinical trial
Talk to your doctor to see if a cancer clinical trial is right for you.
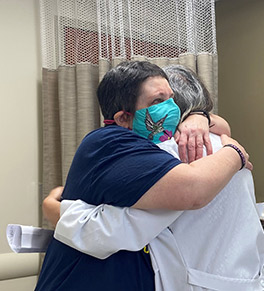
LeeAnn Brill, Breast Cancer Survivor
“I was blessed to get my treatment at UCI Health, where I have received excellent, kind and compassionate care from a wonderful team that treated me as part of their family.”
Featured Blog Posts
Weight loss is better together
Sisters undergo bariatric surgery, drawing inspiration from each other to shed pounds and improve health.

Drummer beats back kidney cancer in clinical trial
Glenn Marquez is hitting the skins again after enrolling in a clinical trial to treat advanced renal cell carcinoma.

A 'dream come true' realized in Irvine
Dr. Michael J. Stamos once envisioned opening a small cancer center on the UC Irvine campus. What has emerged, he says, is so much more.
Types of breast cancer
Our breast cancer team specializes in every type of breast cancer and breast disease, including:
- Benign breast disease
- Breast cancer in men
- Ductal carcinoma in situ
- Gynecomastia
- HER2-positive breast cancer
- Hormone-receptor positive breast cancer
- Invasive ductal carcinoma
- Invasive lobular carcinoma
- Metastatic breast cancer
- Triple-negative breast cancer
Breast cancer treatment at UCI Health
Our breast cancer team will work with you — and each other — to tailor your breast cancer treatment plan to your needs.
Your team will start planning your care at our weekly multidisciplinary breast cancer meeting. During this meeting, our breast cancer experts discuss your care plan together.
The following specialists will all weigh in on your plan:
- Breast cancer surgeons
- Plastic and reconstructive surgeons
- Medical oncologists
- Radiation oncologists
- Genetics specialists
- Pathologists
- Supportive oncology providers (e.g., dietitians, social workers)
- And others
This means you’ll have an entire team of experts determining the best way to treat your breast cancer. That’s like getting a built-in second opinion.
Your treatment plan
After the team meets with each other, your doctors will discuss the plan with you.
Your treatment will likely include a combination of the following treatments:
- Breast surgery
- Medications (e.g., chemotherapy, hormone therapy)
- Radiation therapy
Together, these treatments address the local area where the cancer is, and the effect cancer can have on your body. All combined, these treatments give you the best chance for being cancer-free.
Why choose UCI Health for breast cancer care?
Lymphedema prevention
One concern after breast cancer surgery is the risk of developing lymphedema (swelling of the arm). This may occur if you need to have many lymph nodes removed during surgery. For people at the highest risk, we offer a groundbreaking lymphedema prevention procedure that has decreased lymphedema rates by 80%. This has been a gamechanger for many high-risk people.
Reducing hair loss from chemotherapy
If you need chemotherapy for breast cancer, one common side effect is hair loss. You may have access to a cooling cap (worn during infusions) that significantly reduces chemotherapy-related hair loss. Insurance does not always cover scalp cooling therapy. But a generous donor has covered the cost for anyone who receives chemo at the Pacific Breast Center location.
Nurse navigators
Throughout your breast cancer treatment, a nurse navigator will help you coordinate your care. They’ll guide you through what to expect, answer your questions and set up appointments. And you’ll have a direct number to reach your nurse navigator easily when you need them.
Clinical trials for breast cancer
As a National Cancer Institute (NCI)-designated academic medical center, we lead and participate in clinical trials for breast cancer. That means you may have access to improved treatments for breast cancer that are not yet widely available.
Nationally recognized for quality care
At UCI Health, you’ll have providers who are leaders in breast cancer, state-of-the-art technology and access to clinical trials. We pair all that with strong support, good communication and personalized care. That’s what high-quality breast cancer care looks like in action. And it’s why the American College of Surgeons designated UCI Health as a National Accreditation Program for Breast Centers.
Upcoming Events
6-2 a.m.
Ride, run and walk for cancer research
12-1 p.m. +7 more dates
Mastectomy Support Group — Before and After
The UCI Health Mastectomy Support Group is safe space for individuals who have undergone or are preparing to undergo a mastectomy.
Korean Women's Cancer Support Group
The UCI Health Korean Women’s Support Group provides help and support for Korean-speaking women who are coping with a cancer diagnosis.




